Conditions
Atherosclerosis
Atherosclerosis
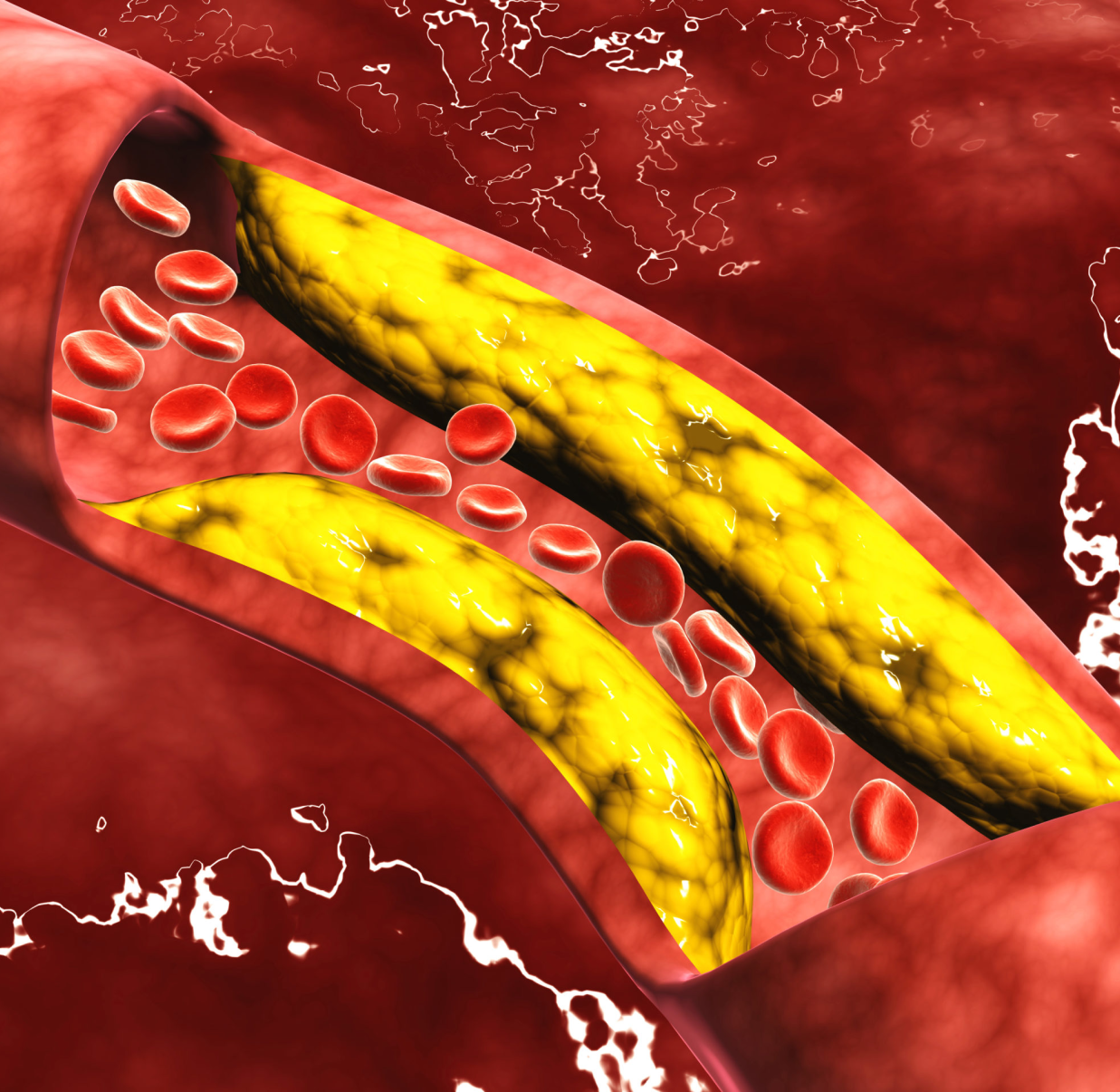
Atherosclerosis is a condition characterized by the gradual narrowing of blood vessels, which play a vital role in distributing blood throughout the body. This leads to a slowdown in blood flow due to the clogged vessels. Larger arteries, responsible for carrying blood away from the heart to various body parts, are particularly susceptible to atherosclerosis. When it affects coronary arteries supplying the heart, it can result in restricted blood flow to the heart muscle, potentially causing a heart attack.
In cases where atherosclerosis obstructs the carotid arteries in the neck, it can impede blood flow to the brain, potentially resulting in a stroke. Atherosclerosis serves as the underlying cause for several related health conditions, including:
Coronary Artery Disease (CAD): Involving blocked arteries in the heart.
Carotid Artery Disease: Involving blocked arteries in the neck.
Peripheral Vascular Disease (PVD): Involving blocked arteries elsewhere in the body, often occurring in the legs, and occasionally in the arms or kidneys.
Atherosclerosis is also known as arteriosclerosis and colloquially referred to as hardening of the arteries.
What is the cause of Atherosclerosis?
Atherosclerosis occurs due to the accumulation of plaque within the arteries, comprising fatty substances such as cholesterol found in your bloodstream. This buildup is a gradual process that unfolds over several years. Over time, the plaque can solidify and narrow the arteries. This condition has the potential to impede or obstruct blood flow, consequently limiting the oxygen delivery to your body tissues.
While cholesterol is a significant factor, other elements can also contribute to atherosclerosis. Several risk factors influence its development. The presence of multiple risk factors increases the likelihood of atherosclerosis.
However, it's important to note that chest pain isn't exclusively linked to reduced oxygen supply to the heart. Sometimes, chest pain may not be angina-related. It could be associated with a pulmonary condition, for example, or simply be a result of indigestion from spicy foods.
Risk factors you can change
- Eating high-fat foods
- Lack of exercise
- Smoking
- Stress
Risk factors you cannot change
- Age-the risk increases with age
- Heredity-the risk increases if there is family history of heart or blood vessel disease
Other health conditions that can increase your risk
- Diabetes
- High blood pressure
To learn more, go to the Risk Factors section and the Health Conditions section (to learn about diabetes and high blood pressure).
What are the Symptoms of Atherosclerosis?
Atherosclerosis manifests differently in individuals. While some may not exhibit any symptoms, others may experience signs of reduced oxygen supply to their tissues, such as:
- Chest pain (angina) stemming from coronary artery disease (CAD)
- Leg pain associated with peripheral vascular disease (PVD)
Feelings of dizziness, numbness, or weakness attributed to carotid artery disease
Erectile dysfunction in men, which may result from artery blockages and lead to difficulties in achieving or maintaining an erection.
What tests could I have?
To determine if you have atherosclerosis, your doctor may recommend one or more of the tests mentioned below. These results will assist your doctor in selecting the most appropriate treatment plan for you. In certain instances, you might be referred to specialists for further diagnosis, testing, and treatment. For additional information, refer to the "Your Treatment Team" section.
- Angiogram
- Ankle Brachial Index
- CT Scan
- Doppler Ultrasound
- Echocardiogram
- Electrocardiogram (ECG or EKG)
- MRI
- Stethoscope Test
- Stress Test
Angiogram
What is an angiogram?
An angiogram is akin to an x-ray image of your blood vessels. It provides crucial information such as:
The efficiency of blood flow through the arteries.
The presence and location of any blockages.
Your doctor might recommend an angiogram if there are suspicions of blockages in:
- Coronary arteries (those supplying your heart).
- Peripheral arteries (those outside your heart).
- Carotid arteries (located in your neck).
The angiogram procedure commences with a cardiac catheterization. This involves the insertion of a small, flexible tube, called a catheter, into a blood vessel in your groin or arm. Your doctor then skillfully guides the catheter toward the blocked blood vessel. Once in position, dye is injected to initiate the angiogram. This dye enables your blood vessels to be visualized on a monitor, much like roads on a map. If the angiogram reveals a blocked artery, your doctor may proceed with a treatment procedure, such as balloon angioplasty, if suitable.
Ankle Brachia! Index (ABI)
What is an ABI?
An ankle brachial index (ABI) is a diagnostic test for peripheral vascular disease (PVD). It involves measuring blood pressure in both your ankle and arm. By comparing these readings, your doctor can identify any blocked blood flow in the arteries of your legs.
The ABI is particularly effective in determining:
The presence of blockages.
The extent of such blockages.
At times, additional tests are conducted concurrently with the ABI. One such test is a Doppler ultrasound. This procedure employs sound waves that bounce off blood vessels and tissues in your leg or foot. This allows for the measurement of blood flow through the specific arteries in that region.
In certain cases, an ABI may be performed in conjunction with a stress test, especially if initial ABI readings are abnormal. The doctor conducts an ABI both before and after the stress test for comprehensive evaluation.
For more detailed information on stress tests or Doppler ultrasounds, refer to the respective entries in the Tests section.
What can I expect?
During an ankle brachial index (ABI) procedure, you'll be provided with a hospital gown to change into. You'll then lie down on an examination table. Blood pressure cuffs will be placed on both arms, and an additional set will be positioned at four points on your legs. These cuffs will be inflated and then gradually deflated, first on your arms and then on your legs. In cases where a Doppler ultrasound is part of the procedure, a gel will be applied to your skin, typically on your feet.
Following the deflation of the leg cuffs, the doctor will glide a pen-like instrument, known as a transducer, over your skin to assess blood flow in the arteries. Much like a standard blood pressure test, the ABI is generally a straightforward and painless examination.
Computed Tomography (CT or CAT) Scan
What is a CAT scan?
A Computerized (or Computed) Tomography (CAT or CT) scan is a specialized form of X-ray imaging. Let's consider its application in examining the heart. While a conventional X-ray provides two-dimensional images showing the heart's length and width, a CAT scan involves an X-ray machine that moves around your body, capturing multiple images of the heart. As small doses of X-rays pass through your body, various types of tissue absorb them differently. This results in a more detailed image compared to a standard X-ray.
The CAT scan images are consolidated on a video monitor, offering a three-dimensional perspective encompassing length, width, and depth. Due to its three-dimensional nature, a CAT scan provides a significantly enhanced view of the entire heart compared to a traditional two-dimensional X-ray.
CAT scans are employed to detect various health conditions, including tumors and bone issues like osteoporosis. In the context of heart and vascular diseases, a CAT scan is frequently utilized to pinpoint:
Certain types of heart conditions, such as heart failure.
Blood vessel obstructions or clots.
What can I expect?
When undergoing a Computed Tomography (CAT) scan, you typically change into a hospital gown or use a sheet for coverage. You lie on an examination table that gradually moves into a machine shaped like a doughnut.
In some cases, you may receive a contrast dye, usually administered through an intravenous (IV) line in your arm. This dye enables your heart or blood vessels to appear as images on a monitor. For example, if the scan is focused on your blood vessels, the dye renders them visible, akin to roads on a map. You may experience some effects from the dye:
A warm, flushing sensation, possibly accompanied by momentary nausea.
A metallic taste when the dye reaches the blood vessels in your mouth.
The technician will instruct you to keep your body still throughout the scan. Sometimes, pillows and/or straps are used to assist you in maintaining the same position. As the X-ray tube revolves around your body, the table slowly moves through the machine. There might be moments when you're asked to hold your breath during the scan. While a CAT scan is generally not painful, you may feel some discomfort from lying in one position during the test, which can last anywhere from 15 to 60 minutes.
Doppler Ultrasound
What is a Doppler ultrasound?
A Doppler ultrasound provides dynamic, three-dimensional imagery of different parts of the body, akin to the ultrasound scans conducted for expectant mothers.
Operating at frequencies inaudible to humans, the ultrasound machine emits sound waves. These waves bounce off the body's fluids and tissues, and the machine records and analyzes how they're reflected back. It discerns even minuscule shifts in each wave's pitch and trajectory. As the waves rebound off the blood vessels, they reveal:
The efficiency of blood flow within the vessels
The presence of any blockages
If blockages exist, their location and extent
Doppler ultrasound captures real-time visuals, including the actual movement of blood through arteries. This enables doctors to identify blockages in various critical areas of the body:
Within the coronary arteries of the heart, where a blockage can precipitate a heart attack
In the carotid arteries of the neck, where a blockage can lead to a stroke
In blood vessels of the legs, potentially causing discomfort due to peripheral vascular disease
This Doppler ultrasound technology is also integrated into echocardiograms, which provide dynamic imagery of the heart.
What can I expect?
During a Doppler ultrasound, you may be asked to partially or fully disrobe and don a hospital gown. Subsequently, you'll recline on an examination table. The technician will apply a gel to the area being examined (such as the neck or leg). This gel facilitates the transmission of sound waves. Using a pen-like instrument known as a transducer, the technician will maneuver it across your skin.
The machine detects the echoes produced by the sound waves bouncing off your body. These echoes are then translated into a dynamic image displayed on the machine's screen: a live depiction of your blood vessels.
While ultrasound is a painless procedure, you might experience some mild discomfort as the sonographer moves the transducer over your body, particularly if a full bladder is required for the examination.
Echocardiogram
What is an echocardiogram?
An echocardiogram, often referred to as an echo, provides a dynamic, three-dimensional view of your heart. It harnesses the power of Doppler ultrasound technology, akin to the ultrasound scans conducted on expectant mothers. The echo machine emits sound waves at a frequency outside the range of human hearing. These waves traverse the chest, passing through the heart. Upon encountering the heart's structures, they rebound or "echo," generating valuable insights into:
The configuration and dimensions of your heart.
The efficiency of your heart valves.
The performance of your heart chambers during contractions.
The ejection fraction (EF), quantifying the volume of blood your heart pumps with each heartbeat.
What can I expect?
During an echocardiogram, you'll be asked to disrobe from the waist up and don a hospital gown. You'll then recline on an examination table. The technician will apply a layer of gel on your chest and side to facilitate the transmission of sound waves. Using a pen-like device called a transducer, the technician will glide it gently across your chest or side. This transducer captures the reverberations of the sound waves. Concurrently, a dynamic image of your heart will be displayed on a specialized monitor. Throughout the procedure, you might be repositioned on your back or side. Additionally, you may be prompted to hold your breath briefly to ensure optimal imaging. An echocardiogram is entirely painless, with only a mild, fleeting pressure felt on your skin as the transducer moves.
Electrocardiogram (ECG or EKG)
What is an ECG?
An electrocardiogram (ECG or EKG) provides insights into the functioning of your heart's electrical system. By sensing and recording your heartbeats or rhythms, it generates a printed record. An ECG serves various diagnostic purposes, including:
Identifying arrhythmias.
Evaluating the effectiveness of your heart medication.
Determining if blocked coronary arteries are impeding blood and oxygen supply to your heart muscle.
Detecting if blocked coronary arteries have led to a heart attack.
There are three types of tests that capture your heart's electrical activity over different durations:
Electrocardiogram (ECG): Conducted in the doctor's office, it records heart rhythms for a few minutes.
Holter monitoring: It logs and stores all heart rhythms over 24-48 hours.
Event recorder: This device continuously records heart rhythms, but stores them in its memory only when you press a button.
What are the parts of an ECG strip?
The electrocardiogram (ECG) strip displays peaks known as waves, collectively offering crucial insights into your heart's performance:
The P-wave indicates the contraction of your heart's upper chambers (atria).
The QRS complex signifies the contraction of your heart's lower chambers (ventricles).
The T-wave represents the relaxation phase of your heart's ventricles.
What can I expect?
During an electrocardiogram (ECG), you'll undress from the waist up and don a hospital gown. Then, you'll lie on an exam table where around 12 small patches, known as electrodes, will be affixed to your chest, neck, arms, and legs. These electrodes, linked to wires on the ECG machine, pick up the heart's electrical signals. Subsequently, the machine records your heart's rhythm on a strip of graph paper.
Magnetic Resonance Imaging (MRI)
What is magnetic resonance imaging (MRI)?
Magnetic Resonance Imaging (MRI) employs a combination of magnets, radio waves, and advanced computing to generate detailed images of various bodily structures, with a particular proficiency in capturing soft tissues. This technique is frequently employed to scrutinize the heart and blood vessels.
During an MRI, you'll be positioned inside a spacious, tube-shaped apparatus. Within the machine, coils generate a potent magnetic field, while other coils emit and receive radio waves. Your body responds by emitting subtle signals. These signals are then detected by the machine, and a computer uses them to construct three-dimensional renderings of your body's interior.
These images can unveil a range of information, including:
Presence of blockages in blood vessels
Dimensions and thickness of your heart's chambers
Areas of muscle damage resulting from a heart attack
Functioning of your heart valves
What can I expect?
Before undergoing a Magnetic Resonance Imaging (MRI) scan, you'll be required to change into a hospital gown or a sheet. Additionally, it's crucial to remove any jewelry, hearing aids, or items containing metal, as the MRI machine employs powerful magnets and having metal objects on your person can pose a risk of injury. Individuals with cardiac devices like pacemakers, implantable defibrillators, or heart failure devices are generally advised to avoid MRI scans. It's imperative for all cardiac device patients to consult their doctor before scheduling an MRI.
Once inside the MRI room, you'll recline on a movable table, and an intravenous (IV) line will be inserted into your arm to administer fluids and medications as necessary. In certain cases, the technician may introduce contrast dye through the IV.
Electrodes, small patches, will be affixed to your chest. These electrodes are linked to wires connected to an electrocardiogram (ECG) machine, which monitors your heart's activity throughout the procedure. Additionally, a blood pressure cuff may be applied to your arm to regularly measure your blood pressure. While the table you're lying on slides into the MRI scanner, the machine itself doesn't have any moving parts. You'll be provided with headphones or earplugs to help mitigate some of the noise produced by the machine, which emits rhythmic thumping sounds. At times, the technician might request that you remain exceptionally still or momentarily hold your breath during specific segments of the test. It's worth noting that you might experience slight muscle twitches in your fingers or toes during the procedure.
Stethoscope Test
Sometimes a very simple test can reveal an artery blockage: your doctor can listen to your blood flow with a stethoscope. An abnormal whooshing sound (called a bruit) as the blood passes through the artery can signal a blockage. A stethoscope test is a good preliminary test. Your doctor may order follow-up tests as well.
What are the treatment options?
Indeed, lifestyle plays a pivotal role in managing atherosclerosis. If you're a smoker, your doctor or nurse can provide information on effective smoking cessation programs that could be tailored to your needs. For additional details, you can refer to the Risk Factors section.
Furthermore, the specific treatments prescribed will be based on the outcomes of your tests. Your doctor may suggest a combination of medications and procedures as part of your treatment plan.
Stress Test
What is a stress test?
A stress test is a specialized form of an electrocardiogram (ECG or EKG) that evaluates how your heart responds to exertion or stress. Unlike regular ECGs, which assess your heart's activity at rest, stress tests focus on its performance under duress. There are various iterations of stress tests, but their primary objective is to ascertain if your heart is receiving an adequate supply of blood and oxygen.
Typically, stress tests are conducted to replicate symptoms like chest pain or breathlessness. The assessment encompasses parameters such as heart rate, blood pressure, and the electrical functioning of your heart. Results from the test can indicate the presence of conditions like coronary artery disease (CAD), the potential for a heart attack, the underlying cause of symptoms like angina (chest pain), and whether irregular heart rhythms (arrhythmias) are present. Additionally, stress tests can help assess the efficacy of treatments, be it medications or implanted devices, in enhancing heart and blood vessel function.
In one of the simpler stress tests, you'll either walk on a treadmill or use a stationary bike. Initially, you start at a gentle pace, and the intensity gradually increases. You'll continue until you experience symptoms or reach a point of exhaustion. This type of stress test is also referred to as an exercise test, treadmill test, or exercise ECG.
During a nuclear stress test, a small amount of a radioactive substance called thallium is introduced into your bloodstream via an intravenous (IV) line, typically in your arm. This substance provides additional insights into whether your heart is receiving sufficient blood and oxygen. While a nuclear stress test is often conducted in conjunction with a regular stress test, it can also be administered if you're unable to exercise, as a medication can be administered to simulate increased cardiac activity.
Following the thallium injection, you'll lie on a table beneath a specialized camera. This camera captures images of your heart. Portions of your heart that receive inadequate blood and oxygen will also receive less thallium, causing them to appear lighter on the images.
What can I expect?
During a stress test, you'll be asked to remove your upper body clothing and put on a hospital gown. Up to 12 small patches, known as electrodes, will be attached to your chest, neck, arms, and legs. These electrodes are linked to wires on the electrocardiogram (ECG) machine, which records the electrical activity in your heart from each electrode. Additionally, a blood pressure cuff will be placed on your arm, and your blood pressure will be regularly checked. If you're undergoing a nuclear stress test, you'll also have an intravenous (IV) line inserted, typically in your arm.
The stress test itself isn't usually painful, although it might replicate certain discomforting symptoms. It's designed to challenge you, and you'll continue exercising until you reach a point of significant fatigue. Throughout the test, a nurse will communicate with you, providing instructions and closely monitoring your symptoms, blood pressure, and heart rate. This monitoring typically continues for about 10-15 minutes after you've finished the exercise.
What are the treatment options?
Given that lifestyle choices can impact atherosclerosis, a crucial aspect of your treatment may involve adopting a healthier way of life. For instance, if you're a smoker, your doctor or nurse can provide information about effective smoking cessation programs. For further details, refer to the Risk Factors section.
The specific treatment you receive will be determined by the results of your tests. Your doctor might suggest one or more of these medications or procedures.
Medications
- Tips for Taking Medications
- Anticoag uIants
- Statins
- Vasodilators
Procedures
- Atherectomy
- Balloon
- Angioplasty
- Bypass Surgery
- Endarterectomy
- Stent Implant
Medications
Tips for Taking Heart Medications
If you have a heart or blood vessel condition, it's important to have a comprehensive understanding of the medications you're prescribed. This section provides details on commonly prescribed medications for heart or blood vessel conditions, along with tips to ensure you take them as instructed.
Remember to inform your doctor, especially if a new prescription is given, about all the medications and supplements you're currently taking. This ensures that you receive the maximum benefits from your medications and helps prevent any potentially harmful interactions between them.
It's crucial to have discussions with your doctor or nurse regarding these topics whenever you're prescribed a new medication:
The purpose of the medication, its anticipated benefits, and potential side effects.
The specific timing and frequency for taking your medications.
Any other medicines, vitamins, supplements, or over-the-counter products you're using.
Patience may be needed as it could take several months for your heart to adjust to new medications. Initial improvements might not be immediately noticeable, and finding the right dosage can also take some time.
For those on heart medications, periodic blood tests might be required. These tests aid in determining the appropriate dosage, thus helping to prevent any adverse effects.
Never alter your medication regimen or dosage independently, even if you think you no longer need it, believe it's not working effectively, or feel well without it.
Remember to communicate with your doctor or nurse if you experience:
Inquiries about how your medications function.
Unpleasant side effects.
Difficulty in adhering to your medication schedule.
Financial concerns regarding your medications.
Any lifestyle challenges that hinder your medication adherence.
Any uncertainties about taking your medications.
Feel free to consult your pharmacist if you have queries about how and when to take your medications.
Anticoagulants (Blood Thinners)
You can understand the purpose of anticoagulants by looking at the root words of the term. Anti = counter or against; coagulant = thicken or clot.
Some Generic (and Brand) Names
All medications are approved by the Food and Drug Administration (FDA) for a specific patient group or condition. Only your doctor knows which medications are appropriate for you.
- aspirin
- clopidogrel (Plavix)
- ticlopidine (Ticlid)
- warfarin (Coumadin)
What They're Used For
To reduce the risk of blood clots that could lead to stroke and other medical conditions
How They Work
Anticoagulants, commonly referred to as blood thinners, don't physically thin the blood. Instead, they work to prevent the formation of clots.
These medications are used to manage conditions associated with atherosclerosis, where arteries are obstructed by plaque. Plaque buildup can lead to the development of a blood clot.
A clot in the coronary arteries (responsible for supplying blood to the heart muscle) can result in angina (chest pain) and is diagnosed as coronary artery disease (CAD), which can lead to a heart attack.
A clot in the carotid arteries (located in the neck) has the potential to travel to the brain and cause a stroke.
Clots in the vessels of the arms or legs, known as peripheral vascular disease (PVD), can lead to pain and related complications.
Anticoagulant medications function by reducing blood stickiness and thereby diminishing the likelihood of blood clot formation.
Statins (Cholesterol Medications)
Statins are commonly called cholesterol-lowering medications.
Some generic (and Brand) names
All medications are approved by the Food and Drug Administration (FDA) for a specific patient group or condition. Only your doctor knows which medications are appropriate for you.
- atorvastatin (Lipitor)
- fluvastatin (Lescol)
- lovastatin (Altocor, Mevacor)
- pravastatin (Pravachol)
- rosuvastatin (Crestor)
- simvastatin (Zocor)
What they're used for
- To lower cholesterol levels
- To reduce the risk of conditions related to high cholesterol:
- Carotidartery disease, which can cause strokes
- Coronary artery disease (CAD), which can cause heart attacks
- Peripheral vascular disease (PVD), which can cause leg or arm pain
How they work
Statin medications have a specific impact on three types of fats in the blood. They function by:
Decreasing the levels of LDL (low-density lipoprotein), often referred to as "bad" cholesterol.
Lowering triglycerides.
Increasing the levels of HDL (high-density lipoprotein), commonly known as "good" cholesterol.
Cholesterol is primarily synthesized by the liver. In individuals with elevated cholesterol levels, the liver produces an excess of cholesterol beyond what the body requires. This surplus cholesterol enters the bloodstream. Statins operate by inhibiting liver cells from generating an excessive amount of cholesterol.
Vasodilators
Vasodilators serve the purpose of reducing blood pressure. To grasp how vasodilators function, envision the same volume of water flowing through a hose with a 1-inch diameter compared to a hose with a 2-inch diameter. The larger the hose, the less pressure exerted on its walls.
Medications like vasodilators aid in the relaxation and expansion (dilation) of blood vessels that have become narrowed (constricted). This process allows blood to flow with less force, thus helping to lower blood pressure.
Some generic (and Brand) names
All medications are approved by the Food and Drug Administration (FDA) for specific patient groups or conditions. Only your doctor knows which medications are appropriate for you.
Here is a list of some vasodilator medications:
Doxazosin (Cardura)
Guanabenz (Wytensin)
Guanfacine (Tenex)
Hydralazine (Apresoline)
Isosorbide dinitrate (Dilatrate, Isordil, Isochron)
Isosorbide mononitrate (Imdur, ISMO, Monoket)
Methyldopa (Aldomet)
Minoxidil (Loniten)
Nitroglycerin (Minitran, Nitro-Bid, Nitro-Dur, Nitrogard, Nitrolingual, NitroQuick, Nitrostat)
Prazosin (Minipress)
Reserpine (Serpalan)
Terazosin (Hytrin)
You may have heard of other types of vasodilators. Beta blockers, which are a common heart and blood vessel medication, are one type of vasodilator. Another type is calcium channel blockers. Always consult with your doctor to determine which medication is suitable for your specific condition.
What they're used for
To treat high blood pressureTo treat/prevent angina (chest pain related to the heart) which can result from atherosclerosis (blocked blood vessels) and coronary artery disease (CAD)
How they work
Vasodilators help relax and dilate the blood vessels, so blood moves through them more easily. This helps to:1. Lower blood pressure2. Allow the heart to work with less effort Decrease the amount of angina (chest pain)
Procedures
Atherectomy
What is an atherectomy?
An atherectomy is a procedure that aims to clear blocked blood vessels by removing accumulated plaque. Typically performed under local anesthesia, it rarely requires general sedation.
This process involves the removal of plaque, facilitating improved blood flow within the artery. This, in turn, can lead to a reduction in:
The risk of a heart attack, especially in the coronary arteries.
The intensity of pain experienced in the legs or arms, particularly in cases related to peripheral artery blockages.
How is the procedure done?
An atherectomy procedure commences with a catheterization. In this step, a flexible tube called a catheter is gently threaded through a blood vessel, typically in the groin or sometimes the arm. The introduction of dye through this catheter enables the visualization of blood vessels on a monitor, akin to roads on a map. This phase, known as an angiogram, is an integral part of the atherectomy process.
Once a clear image of the blockage is obtained, the actual atherectomy begins. Here, a specialized catheter equipped with a small cutting tool is employed. This tool delicately removes the plaque from the inner lining of the artery. Importantly, it is designed to exclusively target the plaque, safeguarding the blood vessel from any harm. With the obstruction removed, blood flow may be restored more effectively.
Following the atherectomy, your doctor may utilize another catheter to insert a stent. This mesh-like tube serves to maintain the openness of the artery, potentially preventing future blockages.
What can I expect?
Typically, you'll be advised to abstain from eating or drinking for a certain period prior to the procedure. The atherectomy is conducted in a specialized room known as the "cath lab". Here, you'll recline on an examination table, and an intravenous (IV) line will be placed into your arm. Through this IV, fluids and necessary medications will be administered during the procedure. These medications induce a state of grogginess, but you won't be fully unconscious.
As the catheter is inserted, the doctor will create a small incision. The area will be numbed, so any pain should be minimal, although you might feel a degree of pressure. Throughout the atherectomy, your doctor or nurse may ask you questions to ensure you're not experiencing any discomfort. While some individuals may stay overnight in the hospital, most tend to recover quite swiftly.
Balloon Angioplasty
What is a balloon angioplasty?
A balloon angioplasty opens blocked blood vessels by pressing plaque against the artery wall. It is a procedure that uses local numbing. General anesthesia usually is not needed.This procedure opens the artery and allows blood to flow more freely, which can reduce your:1. Risk of heart attack-in the coronary arteries2. Level of pain in your legs or arms-in the peripheral arteries3. Risk of stroke- in the carotid arteries
How is the procedure done?
A balloon angioplasty usually commences with a catheterization. In this process, a small, flexible tube known as a catheter is inserted through a blood vessel, typically in the groin or occasionally in the arm. The doctor guides the catheter towards the obstructed vessel. Dye is introduced through the catheter to make your blood vessels visible on a monitor, akin to roads on a map (this step is referred to as an angiogram). Both the catheterization and angiogram are integral parts of the procedure. Once a clear image of the blockage is obtained, the angioplasty commences.
In angioplasty, a specialized catheter equipped with a small balloon at its tip is employed. The doctor inflates the balloon near the blockage within your artery. This inflation presses the plaque against the artery wall, facilitating improved blood flow.
Following the balloon angioplasty, your doctor might use another catheter to insert a stent. A stent is a minuscule mesh tube that maintains the openness of your artery. This intervention can help forestall a recurrence of blockage.
What can I expect?
Typically, you'll receive instructions not to eat or drink anything for several hours before the procedure. The intervention will take place in a specialized room called a "cath lab." You'll recline on an examination table, and a thin tube known as a catheter will be inserted into a blood vessel, often in the groin. This is done after numbing the area to ensure you don't feel pain, though you might experience some pressure as the catheter is introduced. Throughout the angioplasty, your doctor or nurse might inquire about any discomfort to ensure your comfort. While some individuals may need an overnight stay in the hospital, most tend to recover quite swiftly.
Bypass Surgery
What is bypass surgery?
In cases where one or more coronary arteries are obstructed, the heart might not be receiving sufficient blood and oxygen. If a less invasive approach like a balloon angioplasty is unlikely to effectively clear the arteries, bypass surgery may be advised. In this procedure, new routes are established to redirect blood flow around the blocked vessels.
Bypass surgery, technically known as coronary artery bypass graft (CABG), is a form of open-heart surgery that necessitates general anesthesia.
Where are the new vessels from?
During bypass surgery, your doctor will harvest a segment of a healthy blood vessel, often from your chest, arm, or leg. This harvested vessel serves as the new pathway for blood flow to bypass the blocked artery. The selection of the healthy vessel(s) is based on factors such as the size and location of the blocked artery. Generally, doctors opt for one of three options when choosing vessels for bypass:
Internal mammary artery - located inside the chest wall.
Radial artery - extending from the elbow to the wrist.
Saphenous vein - running the length of the leg.
It is medically permissible to remove sections of these blood vessels for bypass surgery because other vessels in the body can take over their functions. Doctors typically prefer arteries over veins for grafts, as veins grafted onto heart arteries can sometimes experience re-clogging, whereas arteries are less prone to this.
How is the surgery done?
In traditional bypass surgery, the procedure commences with an incision made in the breastbone (sternum). This method necessitates the heart to be completely still during the operation. To achieve this, you are administered medications that temporarily halt your heart's activity. A heart-lung machine then takes over the responsibilities of both the heart and lungs:
It oxygenates your blood, akin to the role of your lungs.
It pumps the oxygenated blood back into your body, emulating the function of your heart.
Your doctor grafts one end of the healthy blood vessel just below the blocked artery, and the other end above it. This establishes a new pathway for blood flow, bypassing the obstructed area. This rerouted path is known as the bypass graft. Following bypass surgery, your blood circulates more freely through your coronary arteries, reducing the risk of a heart attack.
A single bypass involves bypassing one blocked artery. A double bypass entails circumventing two blockages, and so forth.
Newer types of bypass
In addition to traditional bypass, some less invasive kinds of bypass surgery now exist. Neither of these two types of surgery uses the heart-lung machine. Your doctor can tell you whether either of these less invasive surgeries might work for you.
Minimally invasive bypass surgery-this requires a smaller incision near your ribs instead of the large incision through the breastbone.
Off-pump bypass surgery- a tool holds part of your heart still while the doctor operates. The rest of your heart beats as usual during this type of surgery.
Bypass surgery outside the heart
While coronary bypass surgery is the prevailing form of vessel bypass, it's worth noting that blood vessels beyond the heart, known as peripheral vessels, can also succumb to blockages. This condition is referred to as peripheral vascular disease (PVD), or peripheral artery disease. In cases of PVD, a bypass procedure may be necessary.
Among the peripheral vessels, those in the legs are most commonly affected. During bypass surgery for leg arteries, the healthy vessel used is either another vessel from the leg or an artificial vessel. Unlike heart surgery, peripheral artery bypass requires general anesthesia but doesn't necessitate the use of a heart-lung machine.
What can I expect?
Before your surgery, you'll typically be instructed to refrain from eating or drinking for a specified period. Once in the operating room, an intravenous (IV) line is established in your arm to administer fluids and necessary medications. Anesthesia is then administered to induce unconsciousness for the duration of the surgery. Post-surgery, you might spend a few days in the intensive care unit (ICU) for close monitoring of your heart function and chest healing. Generally, you can expect to be discharged within a week. While you may experience some discomfort at the incision site for several weeks, pain relief medication will be provided. Recovery at home typically takes around 4-6 weeks.
Following bypass surgery, your doctor might recommend cardiac rehabilitation, which involves a dedicated team of healthcare professionals working with you to facilitate your recovery and minimize the risk of future heart-related issues.
Showsyou the best exercises for you
Suggestsnew eating habits
Ordersmedication to reduce your symptoms
Helpsyou regain or learn new lifestyle and coping skills
Counselsyou on making lifestyle changes (maybe to quit smoking or reduce stress in your life)
Endarterectomy
What is an endarterectomy?
Endarterectomy is a surgical procedure aimed at opening blocked blood vessels by removing accumulated plaque from the inner walls of the artery. This restoration facilitates smoother blood flow through the arteries. Typically, endarterectomy is performed to address plaque build-up in two specific types of vessels:
The carotid arteries in the neck-to reduce your risk of stroke
The peripheral arteries in the legs and arms-to relieve pain
An endarterectomy is a surgery that usually requires general anesthesia.
How is the surgery done?
During an endarterectomy, regardless of the specific location of the blocked blood vessel, the surgical procedure follows a consistent approach.
For instance, when addressing a blocked carotid artery, the surgeon initiates the process by making an incision in your neck. Once the blockage is located, a tube known as a shunt is inserted both above and below the blockage. This shunt serves to redirect the blood flow around the blockage during the surgery. Using a specialized instrument, the surgeon removes the accumulated plaque. After the shunt is taken out, the carotid artery and the incision are carefully sutured closed.
What can I expect?
Typically, you'll be advised to refrain from consuming food or liquids for a specific period before your surgery. Once in the operating room, you'll be positioned on an examination table and an intravenous (IV) line will be inserted into your arm. This IV line serves to administer necessary fluids and medications throughout the surgical procedure. Subsequently, you'll be transported into the operating room. Here, you'll receive anesthesia that induces unconsciousness during the surgery. Following the procedure, you might have a hospital stay of around 12 days. After being discharged, it's crucial to avoid sudden or excessive movements of your neck for the initial couple of weeks.
Stent Implant
What is a stent?
A stent is a minute mesh tube that serves to maintain the openness of an artery. After undergoing an angioplasty procedure, a stent may be implanted in the newly opened artery to lower the risk of recurring blockage or constriction. This is commonly performed in arteries supplying blood to the heart (coronary arteries) or the neck (carotid arteries). The stent implantation procedure involves local numbing, and general anesthesia is typically unnecessary.
Coronary artery stents come in two types: bare metal and drug-coated. A drug-coated stent is essentially a bare-metal stent coated with a specialized medication, designed to reduce the likelihood of the artery re-blocking. This drug coating is gradually released from the stent during the period when a new blockage is most likely to occur.
Opting for a drug-coated stent implant may potentially diminish the necessity for a subsequent procedure (such as another coronary stent procedure or bypass surgery) to re-open the artery.
How is the implant procedure done?
Prior to a stent implantation, your doctor might opt to open the obstructed artery through procedures like an atherectomy or a balloon angioplasty. These interventions, including the stent implant, involve a catheterization. During this process, a pliable tube known as a catheter is inserted through a blood vessel, typically in your groin or occasionally in your arm. Your doctor adeptly guides the catheter toward the blocked vessel. The introduction of a contrast dye through the catheter enables your blood vessels to be visualized on a monitor, akin to roads on a map. This step, termed an angiogram, is usually integrated into the stent implant procedure.
Following the clearance of the blockage, a specialized catheter is employed to position the stent within the newly opened artery. The stent serves two key purposes:
Maintaining the openness of the artery, facilitating unrestricted blood flow.
Preventing the accumulation of plaque that could lead to re-blocking of the artery.
What can I expect?
Typically, you'll receive instructions to abstain from eating or drinking for several hours before the procedure. The intervention will take place in a specialized room known as a "cath lab." You'll recline on an examination table, where a healthcare provider will insert an intravenous (IV) line into your arm. This IV administers essential fluids and medications throughout the procedure. While the medication induces drowsiness, it won't render you unconscious.
The doctor initiates a small incision to introduce the catheter. The area will be anesthetized, ensuring you don't experience pain. However, you might feel some pressure as the catheter is maneuvered. Throughout the stent implantation, your doctor or nurse may ask you questions to ascertain that you're comfortable. It's common to stay overnight in the hospital, and there might be some tenderness at the incision site. Recovery for most individuals is relatively swift.