Conditions
Supraventricular Tachycardia
Supraventricular Tachycardia
Unusual heart rhythms include supraventricular tachycardia (SVT), which is a type of fast heartbeat. Arrhythmia is the term for an unnatural heartbeat. An issue with your heart's electrical system results in an arrhythmia. Your heart contracts because electrical signals travel along a particular path through the heart. However, during SVT, a portion of the heart receives an excessive amount of signals.
A tachycardia is an arrhythmia in which the heart beats (contracts) more quickly than 100 times per minute as opposed to the typical 60–100 beats per minute. SVT is a form of tachycardia that frequently affects the atria, the upper chambers of the heart. SVT can also happen in the tissue known as the atrioventricular (A-V) node, which is located directly above the lower chambers (the ventricles). As a result, the tachycardia is known as supraventricular tachycardia, or above (supra = above) the ventricles.
The atria and ventricles frequently don't have time to fill with blood during SVT before the blood is pumped out of those chambers. Symptoms may result from this.
SVT comes in a variety of particular forms. Most SVT has an abrupt beginning and end. However, SVT can last anywhere from a few seconds to several hours or even longer.
Sinus tachycardia, one type of SVT, is typically regarded as "normal.".
The sinus node, also known as the sinoatrial node, is where sinus tachycardia originates. The sinoatrial node fires off electrical impulses more quickly than usual during sinus tachycardia. Since sinus tachycardia frequently happens during or after exercise, when your heart needs to beat more quickly than usual, it is generally accepted that sinus tachycardia is normal. Sinus tachycardia can, however, occasionally be brought on by a fever, excessive alcohol or caffeine consumption, or a hyperactive thyroid gland. Sinus tachycardia is not handled by itself. But if that.
For instance, the underlying cause may be treated if arrhythmia develops as a result of fever.
What is the cause Supraventricular Tachycardia?
- Bacterialpneumonia
- Chronicobstructive pulmonary disease (COPD)
- Congenital heart problem (a problem present from birth)
- Coronaryartery disease (CAD) (not enough blood supply in heart)
- Damageor death of some heart tissue, which can result from a heartattack
- Diabetes
- Heart failure
- Valve disease
In some cases SVT can lead to rapid arrhythmias in the ventricles- which can be more serious. And in some cases SVT can lead to cardiomyopathy.
What are the symptoms of Supraventricular Tachycardia?
Supraventricular tachycardia (SVT) has a variety of symptoms. Some people experience palpitations, or the sensation that their heart is speeding or that their heartbeat is erratic. Others experience heart pain, weakness, fatigue, sweating, lightheadedness, dizziness, fainting, upset stomach, or decreased appetite. Though SVT often does not pose a life-threatening hazard, the symptoms can be very bad.
What tests could I have?
Since a supraventricular tachycardia (SVT) can be detected by a low blood pressure reading, your doctor may start by doing so. Then, one or more of the below-listed tests may be recommended by your doctor. The outcomes of the test may also aid your doctor in determining the best course of action for you.
You may occasionally be referred to specialists for diagnosis, testing, and occasionally treatment. Visit the section on your treatment team for more information.
- Echocardiogram
- Electrocardiogram (ECG or EKG)
- Electrophysiology (EP)
- Study Event Recorder
- Holter Monitoring
Echocardiogram
What is an echocardiogram?
A three-dimensional, moving picture of your heart is called an echocardiogram, or just an echo. Doppler ultrasonography is used in echos. It is comparable to the ultrasound exam that expectant mothers undergo. The sound waves produced by the echo machine are at a frequency inaudible to humans. The waves flow through the heart and across the chest. The waves "echo" or reflect off the heart, displaying:.
- Theshape and size of your heart
- Howwell the heart valves are working
- Howwell the heart chambers are contracting
- The ejection fraction (EF), or how much blood your heart pumps with each beat
What can I expect?
You strip up to your waist for an echocardiography, put on a hospital gown, and lie on a table. To aid transfer the sound waves, the technician applies gel to your side and chest. The technician will then slide a transducer, which resembles a pen, around on your side or chest. The transducer captures the sound waves' echoes. A moving image of your heart is displayed on a specialized monitor at the same time. Depending on the component of the test you're taking, you might be asked to lie on your back or your side. In order for the technician to acquire a clear picture of your heart, you might also be requested to briefly hold your breath. A test with an echo is painless. You feel only light pressure on your skin as the transducer moves back and forth.
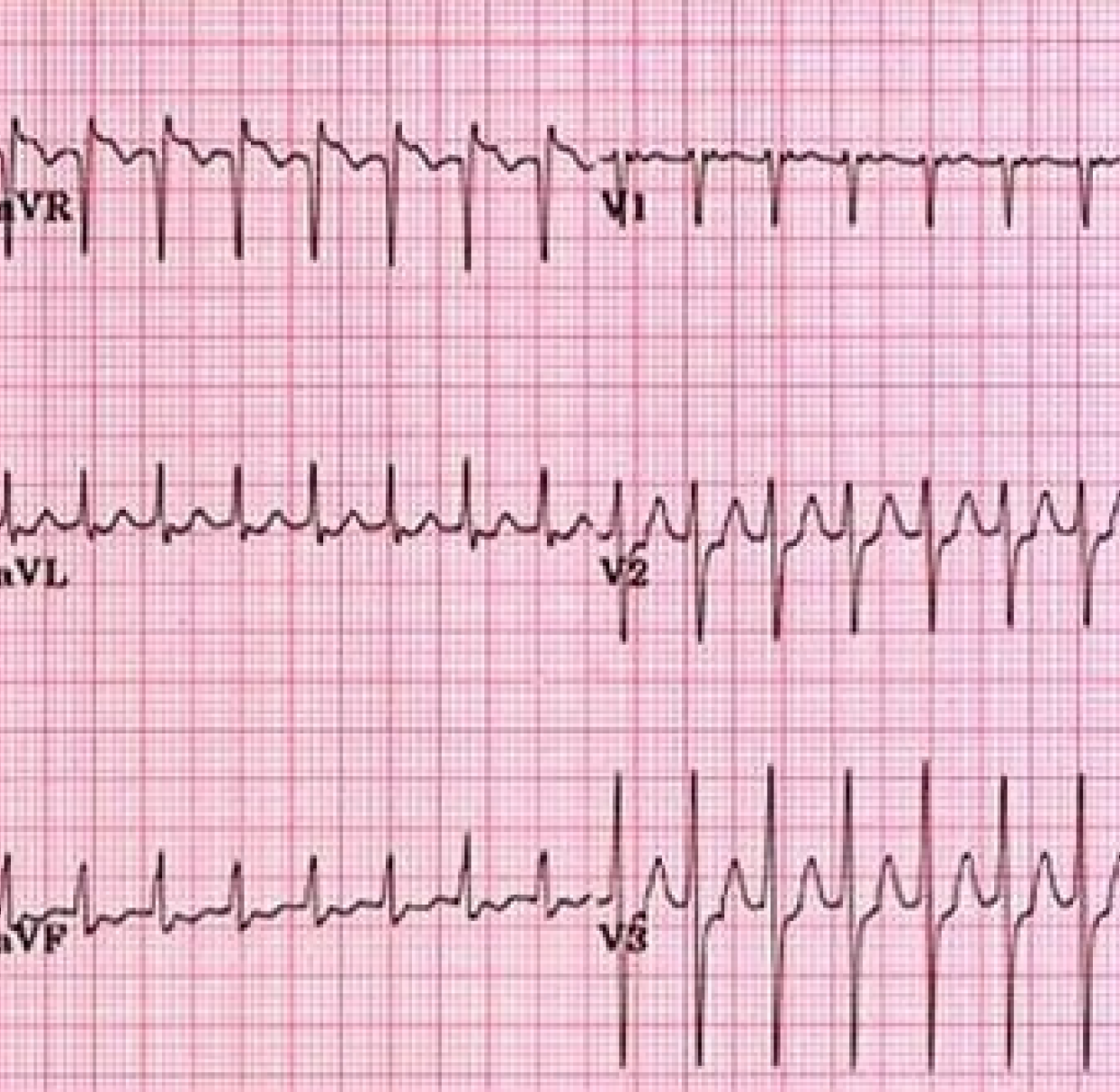
Electrocardiogram (ECG or EKG)
What is an ECG?
An electrocardiogram, also known as an EKG or ECG, shows the electrical activity of your heart. Your heart rhythms, or beats, are detected and recorded by the ECG. A paper strip bearing the results is printed on it. Your doctor can also benefit from an ECG.
diagnose whether:
- Youhave arrhythmias
- Yourheart medication is effective
- Blocked coronary arteries (in the heart) are cutting off blood and oxygen to your heart muscle
- Yourblocked coronary arteries have caused a heart attack
In all, there are three kinds of tests that record your heart's electrical activity, each for a different period of time:
- Electrocardiogram (ECG)-done in the doctor's It records your heart rhythms for a few minutes.
- Holter monitoring– records and stores (in its memory) all of your heart rhythms for 24-48
- Event recorder-constantly records your heart But it stores the rhythms (in its memory) only when you push a button.
What are the parts of an ECG strip?
The peaks on an electrocardiogram (ECG) strip are called waves. Together, all the peaks and valleys give your doctor important information about how your heart is working:
- TheP-wave shows your heart's upper chambers (atria) contracting
- TheQRS complex shows your heart's lower chambers (ventricles) contracting
- TheT-wave shows your heart's ventricles relaxing
What can I expect?
You take off your clothes up to your waist, put on a medical gown, and lie down on a table to have an electrocardiogram (ECG). Your chest, neck, arms, and legs may receive as many as 12 electrode patches. The electrodes on the ECG equipment sense the electrical signals coming from the heart. The device then plots a strip of graph paper with the beat of your heart on it.
Electrophysiology (EP) Study
What is an EP study?
The electrical system of your heart is examined during an electrophysiology (EP) investigation. The EP study provides a more detailed look at your heart's electrical system than an electrocardiogram (ECG) does. The exam aids in learning more specifics regarding irregular cardiac rhythms, or arrhythmias. What the EP study can show is
- If you have an arrhythmia
- The cause of the arrhythmia
- The arrhythmia begins in the heart
- If you are at risk for sudden cardiac arrest (SCA)
- The best treatment for an arrhythmia
One or more leads are inserted into a blood vessel, typically in the groin, to start the EP study. The physician "steers" the leads gently in the direction of your heart. Once in position, the leads detect electrical activity in your heart. An arrhythmia can be brought on by your heart receiving electrical signals from a special lead. That will aid in determining how readily your heart can generate arrhythmias on its own.
Your doctor keeps a close eye on your heartbeat throughout the EP study. If an arrhythmia develops, your doctor will treat you with: Drugs administered through an intravenous (IV) line in your arm or hand Electrical signals applied to the outside of your chest through patches.
Ablation, a type of treatment, may occasionally be carried out concurrently with your EP study. (Visit the Procedures section of the Medications and Procedures section to learn more about ablation. After the EP study, your doctor may also suggest different forms of therapy.
What can I expect?
In a "cath lab," your test will be conducted. "You take off your clothes, put on a hospital sheet or gown, and lie on an examination table. Throughout the test, fluids and medications are given through an intravenous (IV) line that is implanted into your arm. You feel sleepy but not out of it because of the medication. Your chest is covered with patches known as electrodes. While the test is being run, the electrodes are watching your heart's electrical signals. Your blood pressure is routinely taken using a blood pressure cuff on your arm.
For the catheter, the doctor makes a tiny incision, typically in the groin. You will feel no pain because the area around your groin will be numbed, but you might feel some pressure as the catheter is inserted. You might experience a racing or pounding heart if the doctor sends electrical signals to your heart. Because you won't be sound asleep during the test, your doctor or nurse may quiz you.
Afterward, you might spend the night in the hospital, but the majority of patients recover fairly quickly.
Event Recorder
What is an event recorder?
A tiny gadget called an event recorder monitors the electrical activity of your heart. A prolonged period of time—typically a week to a month or longer—is monitored by an event recorder for electrical activity in your heart. The recorder is always on, but it requires a button press to store your heart rhythms in memory. Many heart rate recorders store recordings of your heart rhythm for 30 to 60 seconds prior to and following button push.
Your physician can detect arrhythmias, or irregular heart rhythms, with the use of an event recorder. Even though arrhythmias are uncommon, it is crucial that your doctor be aware of them and treat them.
There are three types of tests in total that capture the electrical activity of your heart, each for a distinct amount of time:.
- Electrocardiogram (ECG)-done in the doctor's It records your heart rhythms for a few minutes.
- Holter monitoring– records and stores (in its memory) all of your heart rhythms for 24-48
- Eventrecorder-constantly records your heart But it stores the rhythms (in its memory) only when you push a button.
Any of these three tests' heart rhythms have the same appearance when written out because the electrical impulses resemble peaks and valleys. When you only experience symptoms once a week or once a month, a doctor might advise an event recorder.
What can I expect?
Your chest will receive two electrodes, which are sticky patches. The event recorder's wires are connected to the electrodes. While the event recorder records and stores the rhythms, the electrodes detect the heartbeats in your body. You will be shown how to remove the electrodes for bathing and then re-apply them by your doctor or nurse. The event recording device is about the size of a tiny portable tape recorder. Putting it in a pocket or on a belt is simple.
When you experience symptoms, you press the button. As a result, only a small portion of the recordings are stored by the device. Make sure your family and friends understand how to operate the recorder as well. They can assist you in pressing the recorder button in case you experience any symptoms. You can send any saved recordings to your physician's office, a clinic, or a hospital. If you need to consult your doctor again, the staff there will let you know.
The event recorder should allow you to complete the majority of your daily tasks at home and at work. While the event recorder monitors your heart rhythms, you won't feel anything. However, the sticky patches can occasionally irritate your skin.
Holter Monitoring
What is Holter monitoring?
The Holter monitor is a tiny recording device used in Holter monitoring. The monitor typically records and tracks the electrical activity of your heart for a period of 24 to 48 hours.
Your doctor can determine if you have arrhythmias, or irregular heart rhythms, with the use of Holter monitoring. Arrhythmias may occur infrequently, but they nevertheless need to be monitored and treated by your doctor.
There are three types of tests in total that capture the electrical activity of your heart, each for a distinct amount of time:.
- Electrocardiogram (ECG)-done in the doctor's It records your heart rhythms for a few minutes.
- Holter monitoring– records and stores (in its memory) all of your heart rhythms for 24-48
- Event recorder constantly tracks your heart But it stores the rhythms (in its memory) only when you push the button.
When the heart rhythms from any of these three tests are printed out, they all appear the same: the electrical signals resemble peaks and valleys. When you experience symptoms at least once every day or every other day, a doctor might advise Holter monitoring.
Any symptoms you experience during the test should be noted by your doctor, who may ask you to do so. Fainting, lightheadedness, or chest fluttering are examples of symptoms.
It's important to keep track of when and how long the symptoms last. Additionally, your doctor might ask you to keep a journal of the times you work out, take medication, or become upset. This can assist your physician in determining whether there is a link between your heart rhythms and your symptoms or activities.
What can I expect?
On your chest, up to seven electrodes—sticky patches—are applied. The electrodes are connected to the Holter monitor's wires. Your heart's rhythms are detected by the electrodes, and are recorded and stored by the monitor. You should take a shower or bath before starting the Holter monitoring, and not at all while the test is being conducted because the electrodes cannot get wet. The Holter monitor is a small portable tape recorder in size. It is simple to wear on a belt or a shoulder strap.
The majority, if not all, of your daily tasks at home and at work should be possible while wearing the Holter monitor. While the Holter monitor records your cardiac beats, you won't feel anything. The monitor must be returned within 24 to 48 hours. The recordings are examined by a technician who creates a report for your doctor after noting any arrhythmias you may have had.
What are the treatment options?
Your treatment depends on your test results. Your doctor may recommend one or more of these medications or procedures.
Medications
- Antiarrhythmics
- Beta Blockers
- Calcium Channel Blockers
- lnotropes
Procedures
- Ablation
- Cardioversion & Defibrillation
- Pacemaker Implant
#
#
Medications
Tips for Taking Heart Medications
If you take any medications, you might be interested in learning more about them if you have a heart or blood vessel condition. This section's content describes a few drugs frequently prescribed for heart or blood vessel conditions. You can use these advice to take your medications as directed.
Make sure to disclose all prescription medications and dietary supplements you are taking to your doctor and any new doctors who will write you a prescription. So that you benefit the most from your medications, your doctor can assist. By sharing this information with your doctor, you can help prevent negative drug interactions.
Each time you receive a new medication, you might also want to bring up these issues with your doctor or nurse:.
- The rationale behind your medication use, any anticipated advantages, and potential negative effects.
- The best times to take your medications.
- If you use any other over-the-counter medications, vitamins, supplements, or other medications.
Sometimes it takes your heart several months to get used to new medications. As a result, it's possible that you won't see changes right away. Your doctor's assessment of the ideal dosage might take some time as well.
People who take heart medications occasionally need blood tests. The blood tests assist your doctor in determining the proper dosage, assisting in the prevention of negative side effects.
Never alter your medication's dosage or stop taking it on your own initiative because you no longer feel the need for it, don't think it's working properly, or feel fine without it.
If you have: be sure to speak with your doctor or nurse.
- Questionsabout how your medications work
- Unpleasantside effects
- Troubleremembering to take your pills
- Troublepaying for your medications
- Otherfactors that prevent you from taking your medications as needed
- Questionsabout taking any of your medications
And don't hesitate to ask your pharmacist if you have questions about how and when to take your medications.
Antiarrhyth mics
The heart's electrical system is impacted by antiarrhythmics. By examining the term's root words, you can learn what antiarrhythmics are used for. Arrhythmia is an abnormal heartbeat or cardiac rhythm; anti is against.
Some generic (and Brand) names
All medications are approved by the Food and Drug Administration (FDA) for a specific patient group or condition. Only your doctor knows which medications are appropriate for you.
- disopyramide (Norpace)
- dofetilide (Tikosyn)
- flecainide (Tambocor)
- procainamide (Procanbid)
- propafenone (Rythmol)
- quinidine (Quinaglute)
Sometimes other categories of medications-beta blockers and calcium channel blockers-are used to help prevent arrhythmias.
What they're used for
- To prevent and treat arrhythmias (abnormally fast or slow heartbeats, or heart rhythms)
- To restore normal heart rhythms
How they work
Antiarrhythmic drugs work in different ways to change the electrical activity in your heart. Different drugs are used because the source of the arrhythmia can come from different places in the heart.
Taking antiarrhythmics can:
- Restore a normal heart
- rhythm Prevent abnormally
- fast rhythms.
Beta Blockers
Beta blockers get their name because they "block" the effects of substances like adrenaline on your body's "beta receptors."
Some generic (and brand) names
All medications are approved by the Food and Drug Administration (FDA) for a specific patient group or condition. Only your doctor knows which medications are appropriate for you.
- acebutolol (Monitan)
- atenolol (Tenormin)
- betaxolol (Kerlone)
- bisoprolol (Zebeta)
- carteolol (Cartrol)
- carvedilol (Coreg)
- labetalol (Trandate)
- metoprolol (Lopressor, Toprol)
- nadolol (Corgard)
- penbutolol (Levatol)
- pindolol (Visken)
- propranolol (lnderal)
- sotalol (Betapace, Sorine)
- timolol (Blocadren)
What they're used for
- to lower blood pressure
- Rapid arrhythmias (irregular heartbeats or cardiac rhythms) to slow
- To avoid angina (chest pain brought on by obstructed blood flow to certain cardiac tissue) To avoid long-term harm following a heart attack
- To treat low ejection fraction (EF), a condition associated with heart failure,
How they work
These drugs prevent your sympathetic nervous system from functioning. When you are under stress or when you have certain medical disorders, your sympathetic nervous system responds. Your heart beats more quickly and forcefully when your body reacts. Additionally, your blood pressure rises.
Beta blockers suppress the sympathetic nervous system's impulses. This lowers your heart rate and prevents the constriction of your blood vessels. These two steps may lead to:
Beta blockers suppress the sympathetic nervous system's impulses. This lowers your heart rate and prevents the constriction of your blood vessels. These two steps may lead to:
- Lower heart rate
- Lower blood pressure
- Less angina (chest pain related to the heart)
- Fewer arrhythmias (abnormal heartbeats, or heart rhythms)
Inotropes
The term "inotrope" describes the force of the heart muscle's contractions or its ability to pump blood.
Some generic (and Brand) names
The Food and Drug Administration (FDA) has given its approval to all drugs for a certain patient population or ailment. The right medication for you is something only your doctor can tell you.
- digoxin (Digitek, Lanoxicaps, Lanoxin)
What they're used for
To lessen the effects of low ejection fraction (EF), which is a condition related to heart failure, and to atrial fibrillation, a rapid rhythm in the upper chambers of the heart.
Calcium Channel Blockers
Calcium channel blockers help relax the heart muscle and blood vessels.
Some generic (and Brand) names
All medications are approved by the Food and Drug Administration FDA for a specific patient group or condition. Only your doctor knows which medications are appropriate for you.
- amlodipine (Norvasc)
- diltiazem (Cardizem, Dilacor, Diltia, Tiazac, Taztia)
- felodipine (Plendil)
- isradipine (DynaCirc)
- nicardipine (Cardena)
- nifedipine (Adalat, Procardia)
- verapamil (Galan, Covera, lsoptin, Verelan)
What they're used for
- To treat high blood pressure
- To treat angina (chest pain) which can result from atherosclerosis (blocked blood vessels) and coronary artery disease (CAD)
- To treat some arrhythmias (abnormal heartbeats, or heart rhythms)- usually fast arrhythmias
How they work
Calcium channel blockers prevent calcium from entering parts of the cells in blood vessels. When calcium is blocked from entering these cells, it relaxes the blood vessels and the heart. As a result, calcium channel blockers:
- Decrease the work of the heart by allowing more blood and oxygen to flow to the heart muscle
- Lower the heart
- rate Lower blood
- pressure
#
Procedures
Ablation
What is ablation?
Targeted areas of the heart muscle are destroyed during ablation. Your doctor picks the areas of the heart muscle that need treatment very carefully. Your doctor will then administer minute amounts of energy to these chosen regions. The heart muscle is left with lesions, which serve as beneficial scars.
Ablation can be carried out using a catheter or as a form of surgery. A flexible tube called a catheter is placed into a blood vessel.
Whether a surgical ablation or a catheter ablation is best for you depends depend on your medical condition. Both catheter ablation and surgical ablation are covered in this section.
Cardiovascular ablation, catheter ablation, cryoablation, microwave ablation, radiofrequency ablation, and surgical ablation are further names for ablation.
How is it done?
Catheter ablation
Chest incisions are not necessary for catheter ablation. Catheterization is the first step in this kind of ablation. A catheter is a tiny, flexible tube that is put through a blood vessel in your groin (or occasionally in your neck) during a catheterization. Your doctor "steers" the catheter into your heart with gentle pressure. Fluoroscopy, which uses moving x-rays or real-time images on a television screen, allows your doctor to see where the catheters are going.
Your heart's electrical activity is sensed and measured by the electrode at the catheter's tip. After checking your heart, a doctor "ablates" it.
utilizing the catheter, cut pieces of the muscular tissue. One method for catheter ablation is:
- Intense cold, called cryoablation
- High-frequency energy, called radiofrequency ablation
In some cases, when ablation is done in certain parts of the heart, you may need a pacemaker afterwards.
Surgical ablation
Six small incisions are needed on the sides of your chest for minimally invasive surgical ablation. The incisions needed for conventional open-heart surgery are substantially larger than these ones (% to % inches in size). Your doctor slips a tiny camera into these incisions to observe the heart. Then, your doctor inserts tiny devices to examine your heart and remove tissue as necessary.
A longer incision must be made through the sternum and along the middle of the chest for open-heart surgical ablation. This kind of ablation is typically performed if you also require another kind of treatment, like a valve replacement or bypass operation.
By providing energy to the heart and producing heat, your doctor can remove portions of the heart muscle using either form of surgical ablation.
- Intense cold, called cryoablation
- Microwave energy, called microwave ablation
- High-frequency energy, called radiofrequency ablation
- Ultrasound energy
- Laser energy
What can I expect?
Usually, you are instructed to refrain from eating or drinking for a period of time prior. In a "cath lab," catheter ablation is carried out. Additionally, an operating room is used for surgical ablation. An IV line is inserted into your arm as you are lying on an examination table. The IV administers drugs and fluids.
The following explanation provides a few specifics regarding each sort of procedure or surgery.
The use of a catheter
The drugs in the IV cause drowsiness but do not render you unconscious. A small incision is made in the groin (or the neck), not the chest, to implant the catheter. You won't feel any pain because the region will be numbed, but you might feel some pressure as the catheter is inserted. Your doctor or nurse may interrogate you while the ablation is taking place. You might spend the night in the hospital afterward.
Surgical ablation with a minimum of pain
You'll be given medication to knock you out during the surgical ablation. Both the ablation itself and the incisions produced on the side of your chest will be invisible to you. You'll likely spend one to two days in the hospital following surgery.
Open-heart surgical ablation
You will be given medication that renders you asleep before the surgical ablation. Both the ablation itself and the cut in your chest will be invisible to you. Spending several days in the hospital following surgery is possible. For several weeks, you can have pain at the incision site. The additional heart surgery you most likely underwent concurrently with the ablation will have an impact on your recuperation.
Ablation References
Fuster V, Ryden LE, Asinger RW, et al., atrial fibrillation. ACC/AHA/ESC guidelines for the management of patients with atrial fibrillation: executive summary, a report from the European Society of Cardiology Committee for Practice Guidelines and Policy Conferences and the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2001;104:2118-2150 in Circulation.
Blomstrom-Lundqvist C, Scheinman MM, Aliot EM, et al., supraventricular tachycardia. The American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines have released ACC/AHA/ESC guidelines for the care of patients with supraventricular arrhythmias. 2003;42:1493–1531. J Am Coll Cardiol.
Scheinman M, Calkins H, Gillette P, et al., Ventricular Tachycardia. Catheter Ablation Policy Statement from NASPE: Personnel, Policy, and Procedures, and therapeutic recommendations. PACE.
2003;26 :789-799.
Cardioversion & Defibrillation
What is cardioversion & defibrillation?
The heart receives an electrical shock from both cardioversion and defibrillation. An irregular pulse can be resumed by the shock. When someone has an arrhythmia—an irregular heartbeat or heart rhythm—they are treated with one of two methods.
Your heart receives a lower-energy shock during cardioversion. Abrupt arrhythmias can be stopped with cardioversion.
An energy-dense shock to the heart is called defibrillation. If the lower chambers of your heart (the ventricles) are experiencing a rapid and chaotic arrhythmia, you need to be treated. When ventricular tachycardia (VT) or ventricular fibrillation (VF) occur, for example, defibrillation is required. The only proven cure for VF is defibrillation. Sudden cardiac death (SCD) can occur rapidly if VF is left untreated.
A similar idea underlies both defibrillation and cardioversion. The heart's electrical activity is temporarily stopped by both forms of therapy. The electrical system of the heart frequently functions properly again once it starts beating again. Go to the section on Heart and Blood Vessel Basics to learn more about the electrical system of your heart.
How is cardioversion or defibrillation done?
An implanted gadget provides internal cardioversion. An implanted cardioverter defibrillator (ICD) is capable of identifying a fast arrhythmia. Next, the ICD shocks the patient with low energy. A normal heartbeat can be restored and the arrhythmias stopped with the shock.
An external device is used to administer external cardioversion. This planned procedure is frequently used to treat fast arrhythmias in the atria, the upper chambers of the heart.
An ICD device provides internal defibrillation. A potentially fatal shock is delivered by the ICD when it detects an arrhythmia such as ventricular fibrillation (VF).
An external defibrillator administers external defibrillation. Most likely, you've watched TV medical dramas with external defibrillators. Two paddles that apply a shock to the outside of the chest are attached to the machine. Defibrillation should be done as soon as possible because brain damage starts to happen four to six minutes after VF starts. Several public buildings and airplanes now have external defibrillators because fast arrhythmias can be extremely dangerous.
What Can I expect?
If there are no symptoms, internal cardioversion or implantable device defibrillation may be unexpected. You may feel cardioversion, but there is no pain. On the other hand, the high-energy shock from defibrillation can be painful. However, arrhythmias such as VF rarely stop on their own. A person must receive treatment to survive. Therefore, defibrillation is generally a life-saving treatment.
External cardioversion is a treatment usually scheduled in a doctor's office. If your atrial arrhythmia doesn't respond to medications, your doctor may recommend them. Remove your clothes and put on a hospital gown or sheet. You will lie on an exam table and an intravenous (IV) line will be placed in your arm. An IV delivers fluids and medications during a short procedure. Drugs make you dizzy, but they don't make you pass out. Your doctor will place patches called electrodes on your chest. The electrodes are connected to wires in the device. The device shocks. Most people report little or no pain afterward.
In emergency situations, external defibrillation is performed. People who receive this treatment usually faint. Chest pain and skin irritation (from shoulder blade) may occur after shock administration.
Pacemaker Implant
What is a pacemaker?
2003;26 :789-799.
A pacemaker is a tiny implantable device used to treat arrhythmias, which are irregular cardiac rhythms. A pacemaker specifically treats bradycardia, a slow arrhythmia. Typically, a pacemaker can cure bradycardia-related symptoms like shortness of breath, exhaustion, and vertigo.
An issue with your heart's electrical system causes arrhythmias. The heart's electrical signals travel along a predetermined course. Your heart contracts due to the mobility of these signals. However, too few signals travel through the heart during bradycardia. Visit the Heart & Blood Vessel Basics section to find out more information about your heart's electrical system.
Your heart's rhythm is returned to normal with a pacemaker. The pacemaker can also change to suit the demands of your body. This is due to the device's sensors' ability to detect:2003;26:789-799.
- When you rest and need a slow heart rate
- When you exercise and need a faster heart rate
It's possible that, for the most part, your heart is effective at controlling your heart rhythm. Only when your heart requires it will a pacemaker be used as a backup treatment.
Other times, a person's heart is no longer able to generate its own electrical signals or direct them along the right channels. Pacemaker therapy, for instance, may occasionally be required due to aging or an ablation procedure in specific areas of the heart. In such circumstances, the pacemaker may administer ongoing therapy to stimulate each heartbeat.
Electricity is sent to the heart by the pacemaker. The system accomplishes this by delivering insignificant electrical energy—too small to feel—either to the top or bottom chambers of the heart, or to both.
The procedure of implanting a device involves local anesthesia. Usually, there is no need for general anesthesia.
An implanted device needs to be checked frequently to review data that is stored there and to monitor settings.
How is the implant procedure done?
A pacemaker system consists of two parts.
It fits easily in the palm of your hand and is quite small. It has tiny computerized components that are powered by a battery.
The wires used to connect the device to your heart are known as leads. They are small, insulated wires. Between your heart and your device, the leads exchange electrical signals.
A small incision, typically located close to your collarbone, is used by your doctor to insert the leads. Your doctor gently guides the leads into your heart and through your blood vessels. Fluoroscopy, which displays moving, real-time x-rays on a video screen, allows your doctor to see where the leads are going.
The doctor attaches the leads to the apparatus and then performs tests to ensure that the two are compatible before beginning treatment. After placing the device just below your skin, your doctor closes the incision with stitches.
What can I expect?
Usually, you are instructed to refrain from eating or drinking for a period of time prior to the treatment. You take off your clothes and don a hospital sheet or gown. You will get your procedure in a "cath lab." An intravenous (IV) line is inserted into your arm when you are lying on an examination table. During the surgery, the IV administers fluids and drugs. You get drowsy but not unconscious from the drug.
To install the leads, the doctor makes a little incision close to your collarbone. You won't feel pain because the region will be numbed, but you might feel some pressure as the leads are introduced. You might spend the night in the hospital, and the incision site might be sore. Most individuals have a pretty