Conditions
Sleep Apnea
Sleep Apnea
Breathing interruptions while you sleep are known as sleep apnea. While you're asleep, your breathing may become very shallow or cease entirely. Most episodes last between 10 and 20 seconds. Some individuals, however, have 30 or more episodes every hour.
Sleep apnea comes in two different forms:
A rare kind of sleep apnea is central apnea. It happens when the area of your brain that regulates breathing is unable to communicate properly with the breathing muscles.
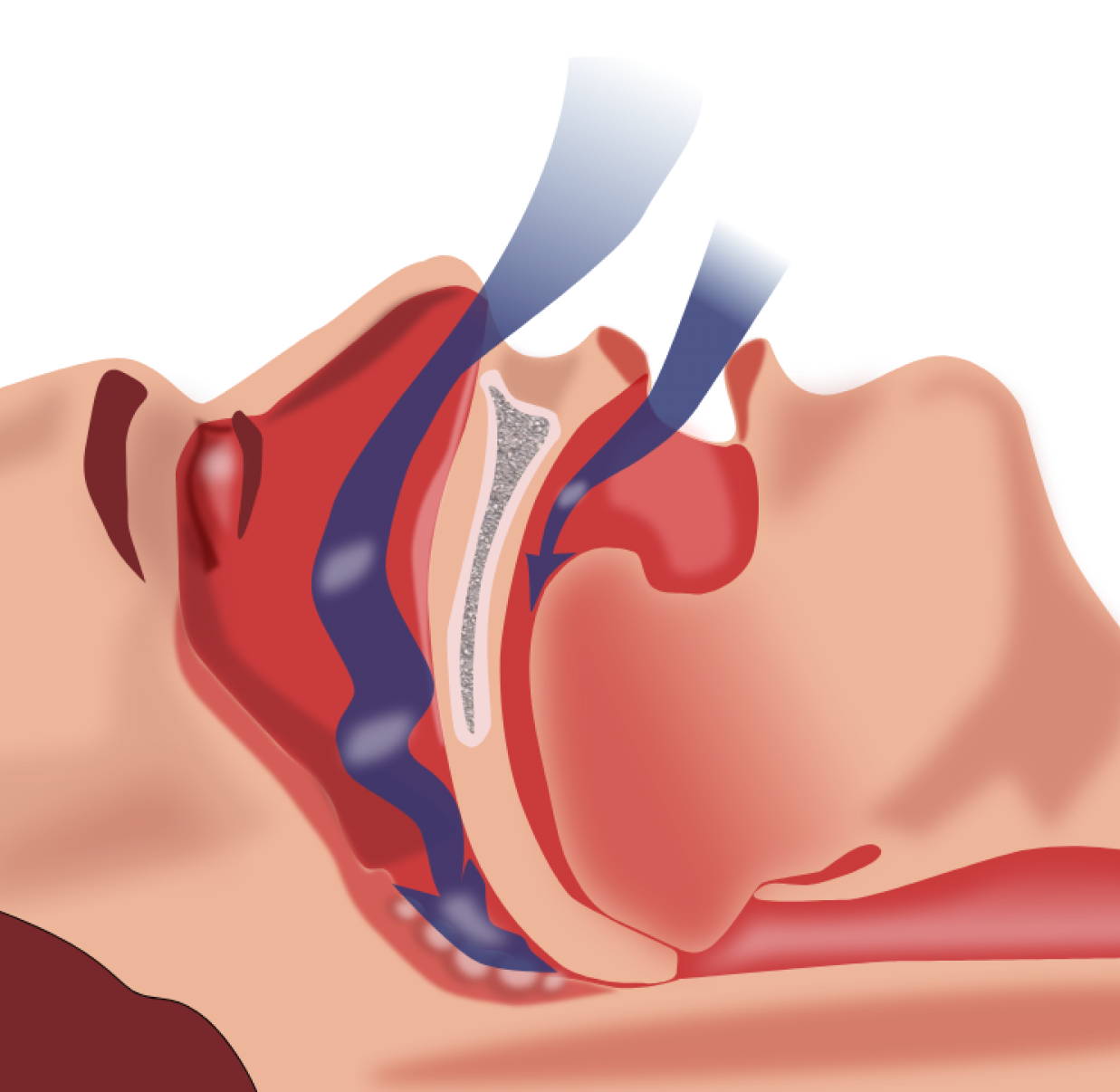
The more prevalent kind of sleep apnea is obstructive sleep apnea. This article addresses this second kind of apnea. It happens when not enough air can enter your lungs through your mouth or nose. The amount of oxygen in your bloodstream may decline as a result. When someone coughs, their breathing usually starts to return.
What is the cause of Sleep Apnea?
Some of the risk factors for sleep apnea are also risk factors for heart and blood vessel disease:
- Excess weight (the extra soft tissue in your throat makes it easier for your throat to close)
- High blood pressure
- Drinking too much alcohol (which can raise blood pressure)
- Smoking
Researchers have also found that people with a certain type of irregular heart rhythm-atrial fibrillation– are more likely to have sleep apnea. Thus there are a number of links between heart conditions and sleep apnea.
There are other risk factors for sleep apnea as well. For instance, it is more common in men. It is also more common in people who:
- Have large tonsils or adenoids
- Have a family history of sleep apnea
- Have smaller airways due to other conditions like allergies
What are the symptoms of sleep Apnea?
Common symptoms include:
- Snoring
- Gasping or choking while sleeping
- Morning headaches
- Daytime fatigue
- Memory problems
- Dry throat
Your sleep partner is frequently the first to detect your sleep apnea symptoms if you exhibit the most typical ones, such as snoring or choking.
What tests could I have?
Your doctor may start with a physical examination of your nose and throat to determine if you have sleep apnea. The next step is frequently a sleep test.
What tests could I have?
Your doctor may start with a physical examination of your nose and throat to determine if you have sleep apnea. The next step is frequently a sleep test.
#
Sleep study
What is a sleep study?
Your breathing, pulse, and brain waves are monitored during a sleep study. To determine if a person has sleep apnea, this test is frequently administered. During a sleep study, the following factors are examined:.
A device tracks your brain waves while you sleep. You apply electrode patches to your head. The electrodes are attached to wires on a machine that monitors the electrical activity in your brain.
- Chin and eye movements are tracked by a device, which reveals the various stages of your sleep.
- (ECGs or EKGs) are used to measure heart rhythm and beat rate. Your chest, neck, arms, and legs are covered in electrodes. The ECG reveals if you experience irregular heartbeats (arrhythmias) while you're asleep.
- Chest bands measure the movements of your chest while you breathe.
The amount of oxygen in your blood is measured by a monitor.
Sleep apnea, which is a disruption in breathing while you sleep, affects your health in what ways? In addition, sleep apnea and conditions like high blood pressure and atrial fibrillation are frequently linked to each other.
What can I expect?
You often spend the night at a specialized sleep center or sleep lab if your doctor instructs you to undergo an overnight sleep study. In a private room, you respond to a series of questions about sleep before going to sleep. Although there are several electrodes on your body, the test is usually painless. Monitors keep track of each of the aforementioned activities as you sleep.
Many of these similar functions are measured by a little monitor that some people bring home. First, a technician walks you through using the home monitoring system. Then you utilize it as you sleep in your own bed at home. The monitored data is examined when it is returned.
No matter what kind of test you undergo, the results will assist your doctor in determining the root of your breathing issues. The results of the test can also help determine how to treat your sleep apnea.
What are the treatment options?
The best ways to treat your sleep apnea will be discussed with you by your physician. The heart and blood arteries are strained by sleep apnea since it reduces your oxygen level while you're asleep. People who have sleep apnea are therefore more likely to experience heart attacks, strokes, heart failure, and sudden cardiac death (SCD).
Medications
Currently there are no medications to treat sleep apnea.
#
#
Other possible treatments
Weight loss
If you have sleep apnea and are overweight, your doctor may suggest that you develop an exercise and diet regimen that works for you. Instead than merely relying on the various treatments described below to treat sleep apnea, it's critical to address this underlying source of the condition.
Procedures
Surgery
Mouthpiece
A specially constructed mouthpiece can be used to treat people with mild sleep apnea. The mouthpiece assists in preventing airway obstruction when you sleep due to your lower jaw and tongue.
Sleeping mask
Sometimes medical professionals advise using a customized nose-fitting sleeping mask. A continuous stream of air is blown into your neck via the mask. The mask works to guarantee that you are receiving all the oxygen you require in this way.
Surgery
On occasion, doctors will advise surgery, such as tonsil or adenoid ectomy. Additionally, more extensive surgery, such as reconstructing the lower jaw, may be required in rare circumstances. Only when weight loss and other treatments fail are invasive procedures advised.